Last year, I wrote about the massive Canadian wildfires that devastated, not only the wilderness, but the air quality in many cities, including New York. Now, reports are coming in of 146 wildfires up north, many out of control, that are causing health issues at the Northern Border such as asthma.
For those who don’t know, asthma is a chronic condition that limits your ability to breathe. It affects the tubes that transport air to your lungs, collectively known as the “airways”. At the time, I didn’t write much about this common but possibly serious consequence of fires. Nevertheless, the family medic should know how to deal with asthma and other respiratory problems, as it affects 20 million Americans and is the most common chronic illness in children.
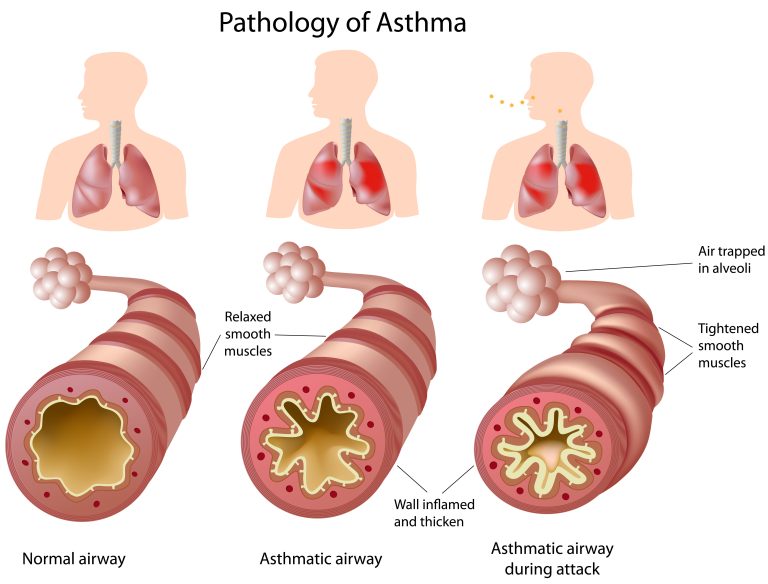
When people with asthma are exposed to a substance to which they are allergic (an “allergen”), airways become swollen, constricted, and filled with mucus. As a result, air can’t pass through to reach the part of the lungs that absorbs oxygen (the “alveoli”).
ASTHMA TRIGGERS
There are many possible triggers for asthma attacks, almost too many to list. They include;
- Pollen
- Pet or wild animal dander
- Mold and mildew
- Smoke
- Dust or the excrement of dust mites
- Aerosol sprays
- Workplace chemicals
- Pollutants in the air
- Some medicines
- Food or food preservatives
In addition, certain viral respiratory infections can trigger asthma, such as respiratory syncytial virus (RSV), COVID, influenza, and rhinovirus (the common cold).
More uncommonly, although generally thought to strengthen the lungs, exercise seems to trigger attacks in some people.
Changes in weather, either hot or cold, is also thought to be a cause. In the fall of 2016, strong thunderstorms in Australia reportedly caused a number of asthma attacks that resulted in hundreds of emergency room visits in Victoria and Melbourne.
PHYSICAL SIGNS AND SYMPTOMS OF ASTHMA
An episode of asthma is commonly referred to as an “asthma attack.” In rare situations, the airways can become so constricted that a person could suffocate from lack of oxygen.
Asthmatic symptoms may be different from attack to attack and from individual to individual. Some of the symptoms are also seen in heart conditions and other respiratory illnesses, so it’s important to make the right diagnosis. Symptoms may include:
- Cough
- Shortness of Breath
- Wheezing (usually of sudden onset)
- Chest tightness (sometimes confused with coronary artery spasms/heart attack)
- Rapid pulse rate and respiration rate
- Anxiety

Besides these main symptoms, there are others that are signals of a life-threatening episode. If you notice that your patient has become “cyanotic”, they are in trouble. Someone with cyanosis will have a blue/gray color to their lips, fingertips, and face.
You might also notice that it takes longer for an asthmatic to exhale than to inhale. As an asthma attack worsens, wheezing may take on a higher, almost musical pitch. As the attack worsens, the patient suffers a lack of oxygen that makes them confused and drowsy; they may possibly lose consciousness.
ASTHMA VS HEART ATTACK
As an asthma attack may resemble a heart attack, the medic should know how to tell the difference. Asthma is usually improved by using fast-acting inhalers, a strategy that doesn’t offer relief from a heart attack or other cardiac events.
Patients with chronic heart disease often have swelling of the lower legs, also called “edema.” This is rarely seen with asthma. Asthmatics also don’t have the arm and jaw pain that is often seen with heart attacks. Cardiac chest pain improves with the angina drug nitroglycerin, which many heart patients carry on their person.
DIAGNOSING ASTHMA

On physical exam, use your stethoscope to listen to the lungs on both sides. Make sure that you listen closely to the bottom, middle, and top lung areas. You’ll find a more detailed discussion of the physical exam in the latest edition of “The Survival Medicine Handbook: The Essential Guide For When Help Is NOT On The Way.”
In a mild asthmatic attack, you will hear relatively loud, musical noises when the patient breathes. Exhaling generally takes longer than inhaling. As the asthma worsens, less air is passing through the airways and the pitch of the wheezes will be higher and perhaps not as loud. If no air is passing through, you will hear nothing even when you ask the patient to inhale forcibly. This person may become cyanotic.
Sometimes a person might become so anxious that they become short of breath and may think they are having an asthma attack. To resolve this question, you can measure how open the airways are with a simple diagnostic instrument known as a “peak flow meter.” A peak flow meter measures the ability of your lungs to expel air, a major problem for an asthmatic. It can help you identify if a patient’s cough is part of an asthma attack or whether they are, instead, having a panic attack or other issue.

To determine what is a normal for an individual, you should first document a peak flow measurement when they are feeling well. Have your patient purse their lips over the mouthpiece of the peak flow meter and forcefully exhale into it. Now you know their baseline measurement. If they develop shortness of breath, have them blow into it again and compare readings.
In moderate asthma, peak flow will be reduced 20-40%. Greater than 50% is a sign of a severe episode. In a non-asthma related cough or upper respiratory infection, peak flow measurements will be normal or close to it. The same goes for a panic attack: Even though they may feel short of breath, the peak flow measurement is still about normal.
Asthma can be fatal if not taken seriously. In the 1980s, I treated a patient in advanced pregnancy who had the worse type of asthma attack, called “status asthmaticus.” Once she improved somewhat, she insisted on going home against my advice to care for her other children. She returned that night in an irreversible state of oxygen loss. Both mother and baby perished.
Next time, we’ll discuss the treatment of asthma with both conventional medicines and with natural means. We’ll also go over some “myths” that should be dispelled (or confirmed!) when it comes to the disease.
via doomandbloom